To try and explain this ever rising trend I underwent a number of MRIs and colonoscopies but nothing untoward was seen and my gastros were stumped. Life continued as usual and my remission appeared to be continuing despite the confusing calpro figures. Could there have been something causing a false positive reading? I set about trying to find a plausible answer (that didn’t involve inflammation) but without success. In the meantime I was wondering why my Hb level was on the low side. Cue another graph…

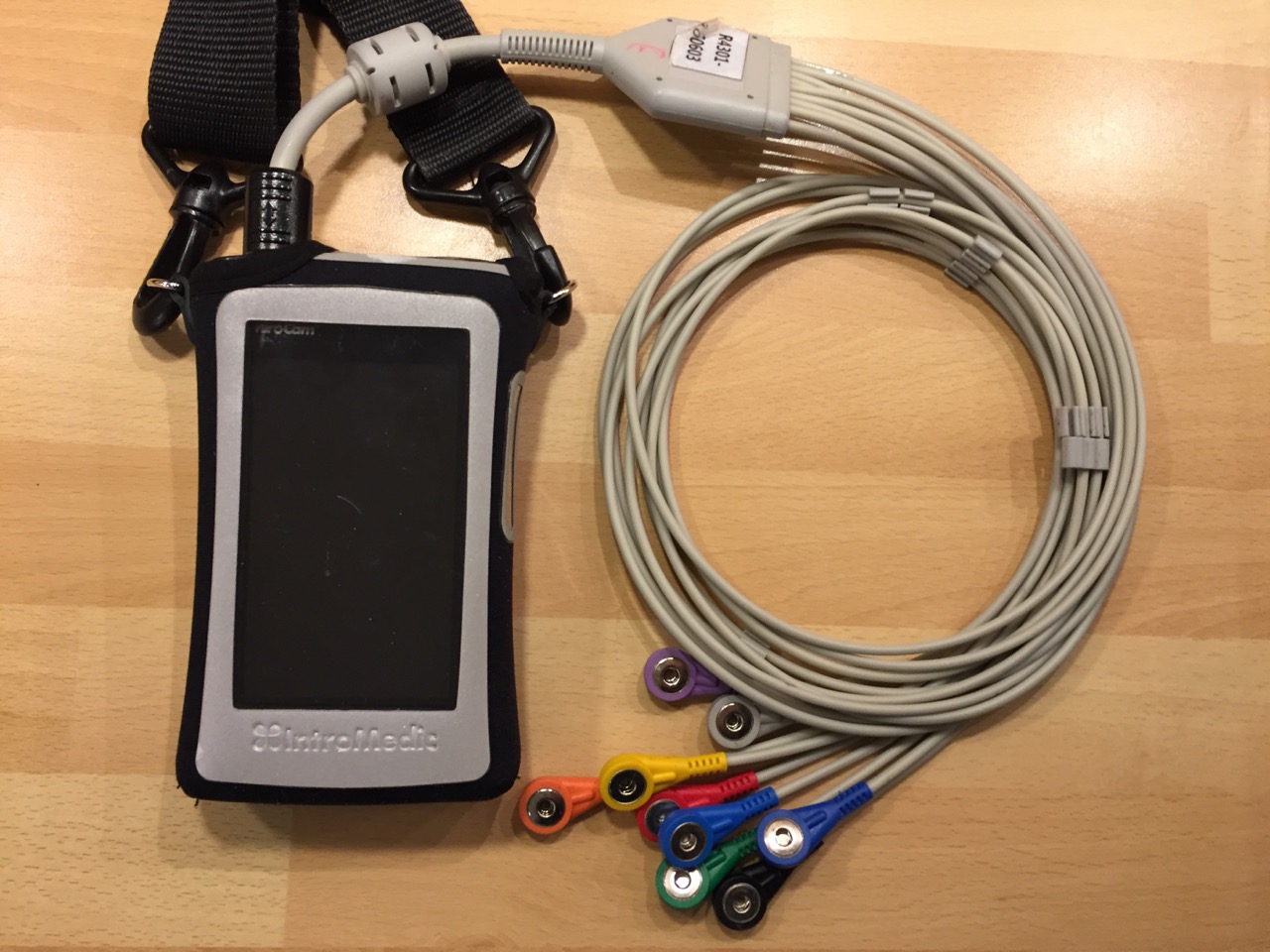
It wasn’t until late 2018 that I went to see my gastro again, ostensibly to discuss the Hb level and a recent bout of “bathroom dashes”. Was it time to re-investigate the calprotectin issue. There was one section of my gut that hadn’t been seen by camera, namely the small bowel between duodenum and the anastomosis site (where my terminal ileum had been). I was booked in for a capsule endoscopy on 18th November. The full description of the procedure and the wait for the results can be found here (opens in a new window) – https://www.wrestlingtheoctopus.com/fantastic-voyage/ .
When the report was finally available my consultant emailed me to say that “there is some inflammation in the small bowel – it’s not terrible but it must be the source of the calprotectin. I think it is probably enough to warrant treatment which we should discuss. Shall I arrange an appointment?” Yes, that would be a good idea. The date has come through for mid-April. A few more weeks wait before finding out the way ahead….
Then, last Thursday, I was rather surprised to get a phonecall from one of the IBD nurses. She told me that it had been decided, at the weekly virtual clinic (which I think must be like an MDT), to start me on Vedolizumab and they needed to book me in for a blood test and chest x-ray prior to my first infusion. I explained that this would be a major decision, as I had been Crohn’s drugs free for several years. My preferred option was to stay that way. I would want to discuss any new drug/treatment, at the forthcoming gastro appointment, prior to starting. (I have subsequently had an email from my consultant agreeing with this course of action. It appears that the IBD nurses had been very efficient in trying to arrange approval for the drug prior to the appointment)
Bluff
I’m now in a position that many other patients are confronted with – the end of remission. I’ve written many times about maintaining a laid back, positive attitude. Now my bluff is being called and I need to prove to myself that I can continue being calm and unstressed about my health. So far so good. If my quality of life was being seriously compromised and I was unable to function properly then the decision to restart medication would be a simple one…..but it isn’t apart from…..
….an ache in my right hand side (URQ). It’s more annoying than being anywhere near painkiller territory. What could be causing it? As with most things #IBD related there is always a high degree of uncertainty. I consider this to be one of the major psychological burdens we bear.
I’m currently testing an IBD Self Help programme. It is broken down into modules which are completed over a number of weeks. I haven’t reached the “Pain” section yet so I’ve been relying on the old technique of visulaising the pain in an attempt to lessen its impact. That’s easier to do if you know there is only one cause but in my case it could be : the recurrence of the old ache around my anastomosis due to adhesions/scar tissue; gallstones; getting the balance of Loperamide/Colesevelam wrong; or the new kid on the block – inflammation. (“New” may be an incorrect description given that the first high calprotectin values showed up in May 2016).
Jump
You might think that I would jump at the chance of starting treatment but I’m not so sure. If inflammation did restart in 2016 then I have thrived so far without medication, do I really need to start now? I don’t want to be dogmatic and take a “I’ve been taking no drugs so I’m not going to start now” stance without good reason. A fellow Crohn’s patient asked what made me hesitant? I suppose the answer is “side effects”. I have not needed to educate myself on the progress of the MABs/biosimilars and their potential downsides. I have a lot of catching up to do and need to understand how the benefits would outweigh the risks.
I have however had experience of drugs damaging other systems or not working. I took Azathioprine for 9 years, with no apparent side effects, then my platelet count suddenly plunged. The concensus was that the Aza had attacked and permanently damaged my bone marrow which in turn reduced its ability to produce platelets. No more Azathioprine. I then tried Infliximab but after 3 doses my symptoms showed no improvement and I went under the surgeon’s knife (2010).

Before the mid-April appointment I need to research Vedolizumab; ask other Crohn’s patients for their experiences and come up with a list of questions for my gastro. I’ve made a start……
Questions, questions….
I would usually leave my list until a couple of days beforehand. Given that this will be a major decision point in my Crohn’s experience I thought it best to start writing now.
- What exactly did the capsule endoscopy show in the way of severity of inflammation and locations? Was it confined to the small bowel?
- What was the gist of the discussion that resulted in proposing Vedo?
- My QOL is good apart from an ache on my right side
- Looking at the calprotectin levels it suggests that inflammation started somewhere between November 2015 to June 2016 but was not apparent on other tests
- It has been 6 months between having the capsule endoscopy mid-November and the appointment. That suggests it does not need immediate treatment.
- What if I decide not to go back onto Crohn’s medication at present?
- How will Vedo help me now? …and in the long term?
- Are there any side effects I need to know about? Are any of these relevant to my other conditions?
- Ongoing monitoring regime? Frequency?
- How good a measure would calprotectin be for small bowel Crohn’s?
- Does the efficacy of Vedo differ as one gets older? Do the side effects change?
- Is there the opportunity to have infusions at a local hospital?
- Was there anything else of note from the capsule endoscopy? Could anything account for my low Hb?
- What can we do about Hb level and long term use of Ferrous Fumarate? Would an iron infusion be the answer?
(If I have missed something obvious or you have beem in a similar situation then please leave a comment or respond on Twitter @crohnoid – Thanks)